Age spots are small areas of discolouration (hyperpigmentation) that affect the face, hands and other areas frequently exposed to sun. They are most common in people over the age of 40, but they can occur earlier is some cases.
The triggers and available treatments for age spots
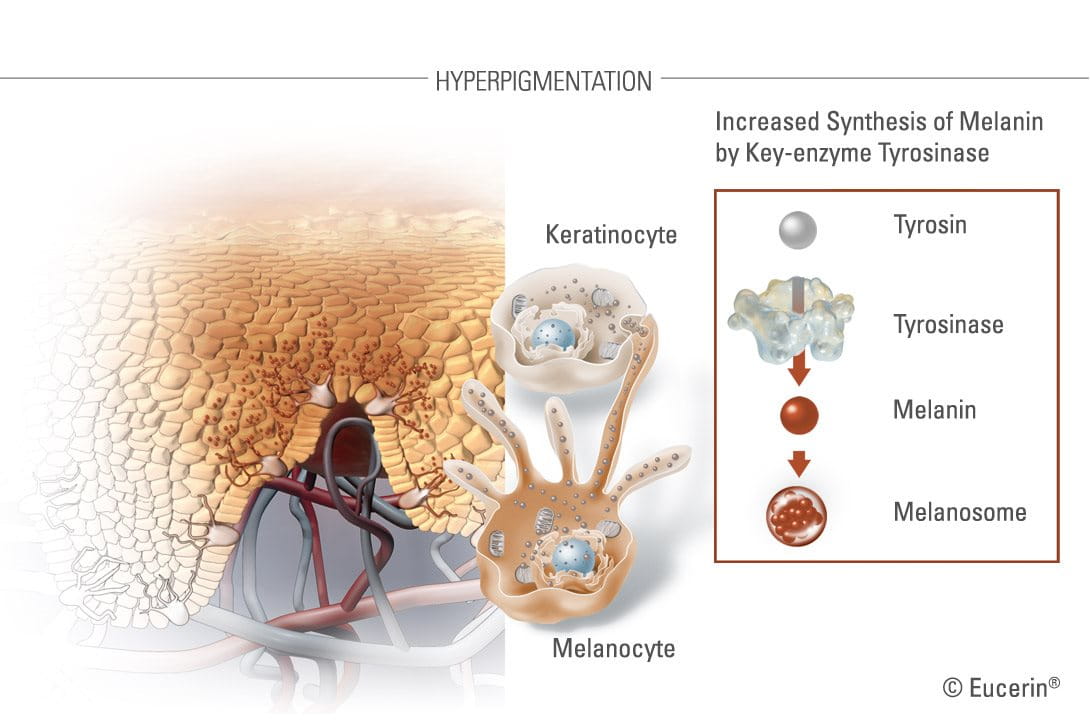
Hyperpigmentation is a common condition whereby melanin – a natural pigment in skin – is overproduced causing dark spots and uneven skin tones. Hyperpigmentation can affect the skin colour of people of any skin complexion though it is more frequent in people of darker skin types. There is no gender bias.


There are many reasons why someone may develop hyperpigmentation, including over-exposure to UV-sunlight, genetic disposition, age, hormonal influences, inflammation or injury. There are several hyperpigmentation disorders, one of which is pigment spots.
Age spots (lentigo senilis or lentigo solaris) are a form of pigment spots.
Usually found on the hands, face and décolleté, or other areas frequently exposed to the sun, age spots are small, flat, darkened patches of skin (light brown to black in colour). They tend to appear on areas of skin that are most exposed to sun, such as the back of the hands, face, forearms, forehead and shoulders. The appearance of pigment spots can make sufferers feel less self-conscious, particularly given their association with ageing.
Although pigment spots are usually harmless certain forms can be life-threatening, as in the case of melanoma. Therefore a regular dermatological assessment of the skin for pigment spots is advisable.
Attention
If a pigment spot is changing in size, shape, colour, or is itching or bleeding, a dermatologist should be visited in order to rule out malignancy.

Melanin absorbs the UV-radiation of the sun’s rays in order to protect the skin. Provided sun exposure is limited, the result is an even tan.
However, if skin is exposed to too much sun, over a long period of time, the activity of melanocytes will increase and too much melanin will be produced. The result will be the appearance of age spots on the most commonly exposed areas, such as the face, hands and décolleté.
As skin ages, the number of melanocytes decreases but the remaining ones increase in size and their distribution becomes more focussed.
Regulation of the melanosomses also becomes less controlled. These physiological changes explain the increase of age spots in those over 40.
Finally, genetics can play a part in the development of age spots. If a parent or parents had age spots, there is a higher chance of them occurring in the next generation.
What causes age spots?
Pigment spots are caused by increased activity of melanocytes, the melanin-producing cells located in the basal layer of the epidermis. The major determinant of skin colour is not the number, but rather the activity of these melanocytes.
Within the melanocytes are pigment granules, called melanosomes, which contain tyrosinase (the pigmentation enzyme that is key to the melanin production) and synthesised melanin. These are transported from the melanocytes to keratinocytes – at approximately 30 keratinocytes per melanocyte.
What treatments exist for age spots?
There are two main concepts used by dermatologists: removal of the skin discolouration caused by hyperpigmentation and regulation of the signs.
In the case of removal, by chemical peel or laser therapy, each can have side-effects, such as irritation, inflammation and even burning, which can actually trigger post-inflammatory hyperpigmentation, especially on darker skin tones. They can also be expensive and invasive.
Removal

Chemical peels eg. AHA
This involves an acidic solution (Glycolic Acid (AHA)) being applied to the affected area to remove the surface layers of skin. The procedure initially leads to blistering. Once the blister peels, new and evenly pigmented skin is revealed underneath.
Laser therapies (Fraxel, Erbium YAG) and Intense Pulse Light (IPL)
Similar but more precise treatments are available using laser therapy. Here the dermatologist ‘zaps’ the affect areas with a high-energy light. Depending on the severity, the light will work on the surface layer (epidermis) or penetrate into deeper layers of skin.
Regulation
A number of topical medical or skincare products are also available to regulate pigmentation. Most rely on one or more of the following key ingredients to lighten the darkened skin patches, to match the normal skin colouration, and/or slow down the production of melanin:
- Hydroquinone 2-4% (Rx only) is a powerful prescription-only skin bleaching agent that has been banned in cosmetics in the EU since 2001 due to its potential toxicological risks and its likelihood of causing post-inflammatory hyperpigmentation. It is available in lower concentrations (>2%) in some US over-the-counter remedies.
- Kojic Acid. A snatural option and a by-product of the Japanese rice wine, sake. However, it is thought to be a fairly weak inhibitor of melanin production and is also banned in many countries.
- Glycolic Acid. As well as being used by dermatologists for chemical peels, Glycolic Acid is an active ingredient in many hyperpigmentation topical creams.
- Vitamin C derivatives. Often used in conjunction with other active ingredients, these derivatives have proven to be relatively effective against hyperpigmentation.


As well as regulating pigmentation, there are ways to prevent the occurrence and key ingredients to reduce the appearance of hyperpigmentation.
- Sun protection. To prevent any further hyperpigmentation, it is advisable to use a broad-spectrum sunscreen with SPF every day as part of a daily cleanse, clear and care routine.
- Arbutin. This natural source of hydroquinone is a key ingredient in many skin-whitening products used in Asia. Although it is not as strong, or effective, as industrially-produced hydroquinone, there are similar concerns about its safety.
- Retinoids (Vitamin A derivatives). Again, these are relatively effective but both can irritate skin and lead to greater sun sensitivity (which, of course, can worsen hyperpigmentation). Retinoids are not considered suitable for pregnant or breastfeeding women due to potential links with birth defects.
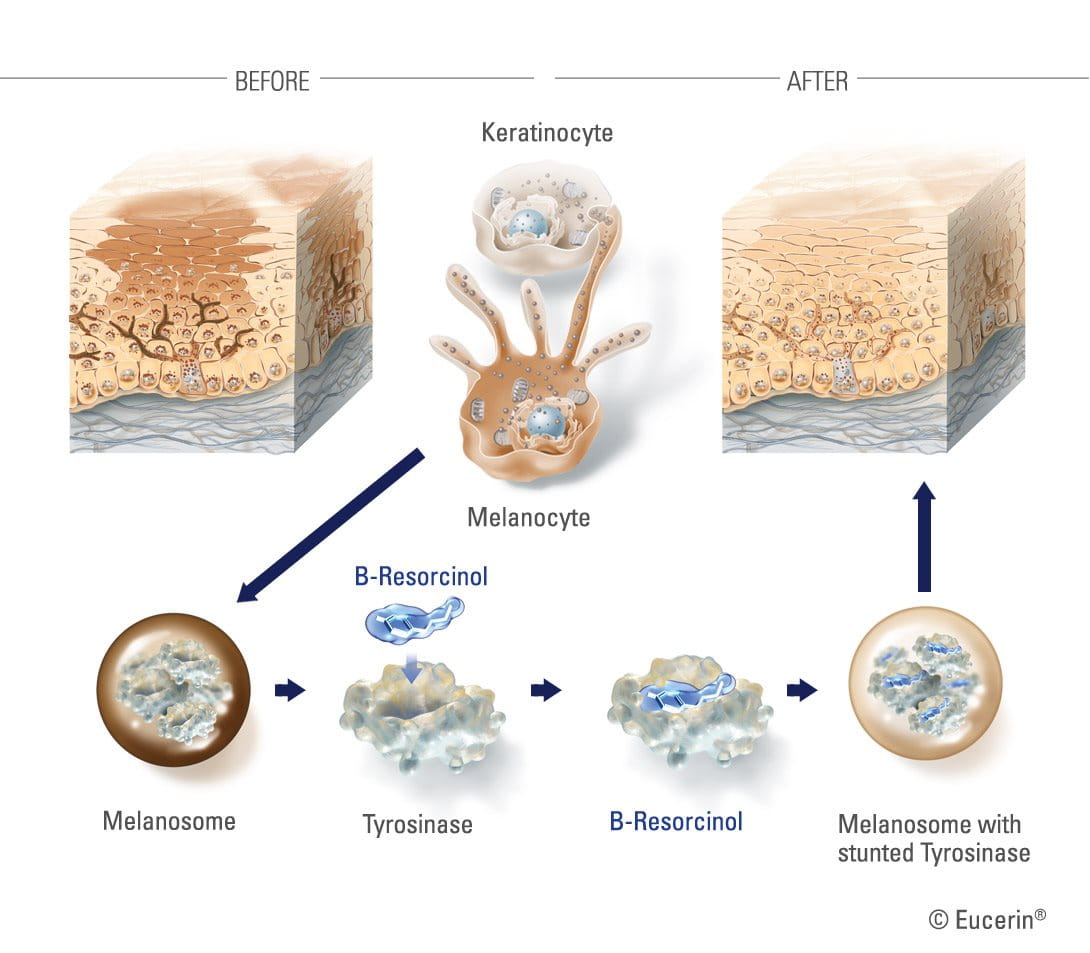
B-Resorcinol
A very effective ingredient in reducing melanin production – and the main active ingredient in the Eucerin Even Brighter range – is B-Resorcinol or butyl resorcinol. It is a very strong inhibitor of tyrosinase (the enzyme that forms melanin) and has been clinically proven to start reducing dark spots in four weeks. It causes little to no skin irritation and is effective against the major kinds of hyperpigmentation like melasma and age spots.
It is important to point out that no overnight results can be expected for hyperpigmentation. It will take time for signs to improve.
Attention
Talk to your dermatologist or pharmacist if any of your dark spots are new, have changed in appearance, or look different to your other spots.



