Melasma is a type of hyperpigmentation that is common in women, especially during and after pregnancy. It appears as large dark patches of discolouration on the face although other parts of the body can be affected.
The signs, causes and available treatments for melasma
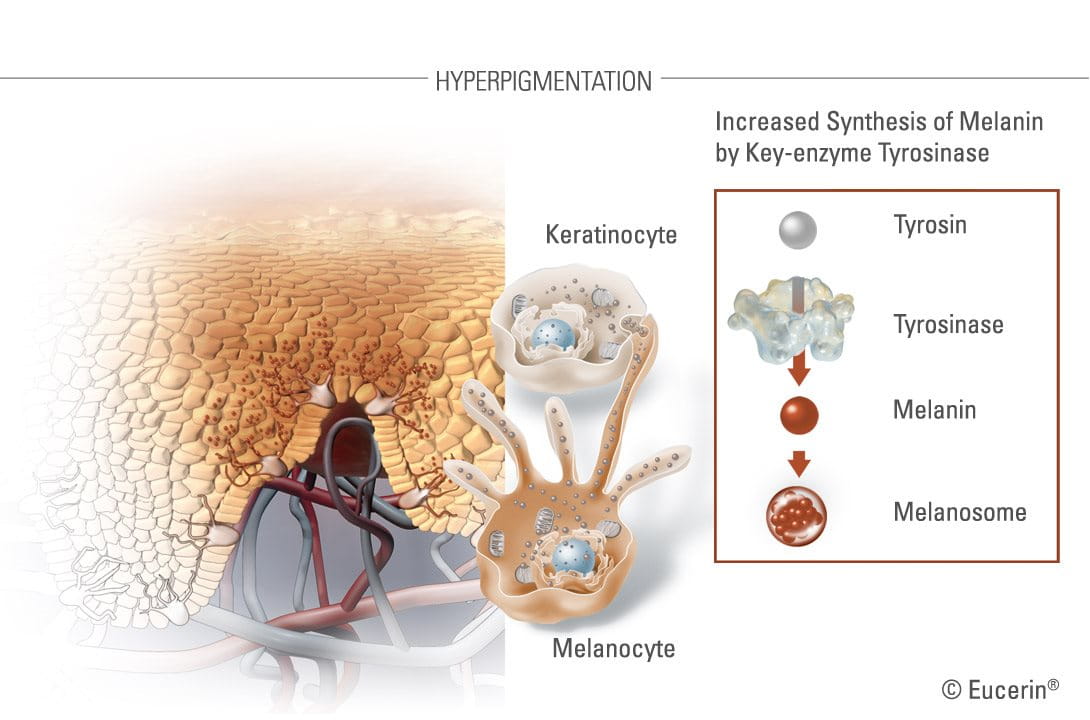
The pigment melanin defines the colour of a person’s eyes, hair and skin. Certain internal and external factors, such as exposure to the sun, genetics, hormonal changes, inflammation and age can affect the production of melanin. Over-production leads to hyperpigmentation, whereby dark spots and uneven skin tones appear. Under-production - hypopigmentation – has the opposite effect, with pigment-free spots developing in affected areas.
Melasma is a form of hyperpigmentation that appears on the face, especially on the cheeks, bridge of the nose, forehead and upper lip and sometimes on other sun-exposed parts of the body, such as the forearms.


There are three types of melasma: epidermal, dermal and mixed.
- Epidermal melasma affects the top layer of skin and the hyperpigmentation is brown with well-defined borders.
- Dermal melasma affects the deeper dermis level and is characterised by blue-gray patches.
- Mixed melasma (a combination of epidermal and dermal) shows as a brown-gray pigment. Due to the depth of the melanin pigments in dermal and mixed melasma, these types can be harder to treat.
Melasma is most common in women – only 10% of cases are male - affecting up to 90% of pregnant women.
For that reason it is also known as “the mask of pregnancy” (or chloasma). While all ethnics are affected, people with darker skin tones are more prone. Unlike age spots, melasma can disappear of its own accord after birth, or if oestrogen intake is reduced.
Attention
If a pigment spot is changing in size, shape, colour, or is itching or bleeding, a dermatologist should be visited in order to rule out malignancy.
What causes melasma?
Melasma is caused by the over-production of the pigment melanin. Whilst the condition usually occurs as a response to hormonal changes, such as pregnancy, birth control pills or hormone replacement therapy (HRT), other factors such as UV-exposure, family predisposition, age and certain anti-epilepsy drugs can also play a role.
Melanocytes (the melanin-producing cells located in the basal layer of the epidermis) are responsible for increased epidermal pigmentation in melasma.
During pregnancy endogenous hormones stimulate the melanocytes, causing them to produce more melanin pigments.
Women who take birth control pills or hormone replacement therapy (HRT) may also develop melasma because their organisms undergo similar kinds of hormonal changes as those that occur during pregnancy.
UV-exposure is also a major triggering or aggravating factor in the development of melasma so it is recommended that people who are prone to the condition, or whose families have a predisposition to melasma, avoid the sun and apply broad-spectrum high-factor sun protection to avoid stimulating pigment production.
What treatments exist for melasma?
There are two options available to sufferers of melasma – removal of the discoloured skin or regulation of the pigment.
Removal


Removal is done by laser therapy, intense pulse light or chemical peel. These can be expensive and invasive and can actually trigger post-inflammatory hyperpigmentation, especially on darker skin tones. Potential side effects include inflammation, irritation and a burning sensation.
Laser therapies (Fraxel, Erbium YAG) and Intense Pulse Light (IPL)
More precise than chemical peels, laser therapies use high-energy lights to target affected areas. This deletes hyperpigmented skin cells, at surface (epidermis) level or deeper (dermis), depending on the severity of symptoms.
Chemical peels eg. AHA
With chemical peels the dermatologist applies an acidic solution (Glycolic Acid (AHA)) to treat the affected layers of skin. Skin tends to blister, then peel, revealing unblemished skin beneath.
Regulation
Alternatively, to regulate skin colouration, a number of topical medical or skincare products have also become available in recent years. These usually contain one or more of the following ingredients:
- Hydroquinone 2-4% (Rx only) - a powerful skin-bleaching agent that is banned in cosmetics in the EU due to concerns over links to potential toxicological risks. It is, however, still used in the US. Higher concentration (Rx >4%) is prescription-only while lower concentrations (>2%) are used in over-the-counter remedies.
- Arbutin. This natural source of hydroquinone is a key ingredient in many Asian skin-whitening products. Although it is not as strong, or as effective, as industrially-produced hydroquinone, similar concerns about its safety exist.
- Glycolic Acid (or hydroxyacetic acid) is used by dermatologists for chemical peels and is a common active ingredient in many hyperpigmentation topical creams.
- Kojic Acid. A by-product of the Japanese rice wine, sake Kojic Acid is a natural ingredient although its ability to inhibit melanin production is debateable and the ingredient is banned in many countries.
- Vitamin C derivatives have proven to be relatively effective against hyperpigmentation and are often used in conjunction with other active ingredients.
- Retinoic Acid has been seen to be effective but can trigger some side-effects including irritation and increased sun sensitivity (which is already an issue for people with post-inflammatory hyperpigmentation). As there have been some potential links to birth defects, pregnant or breastfeeding women should not apply Retinoic Acid.
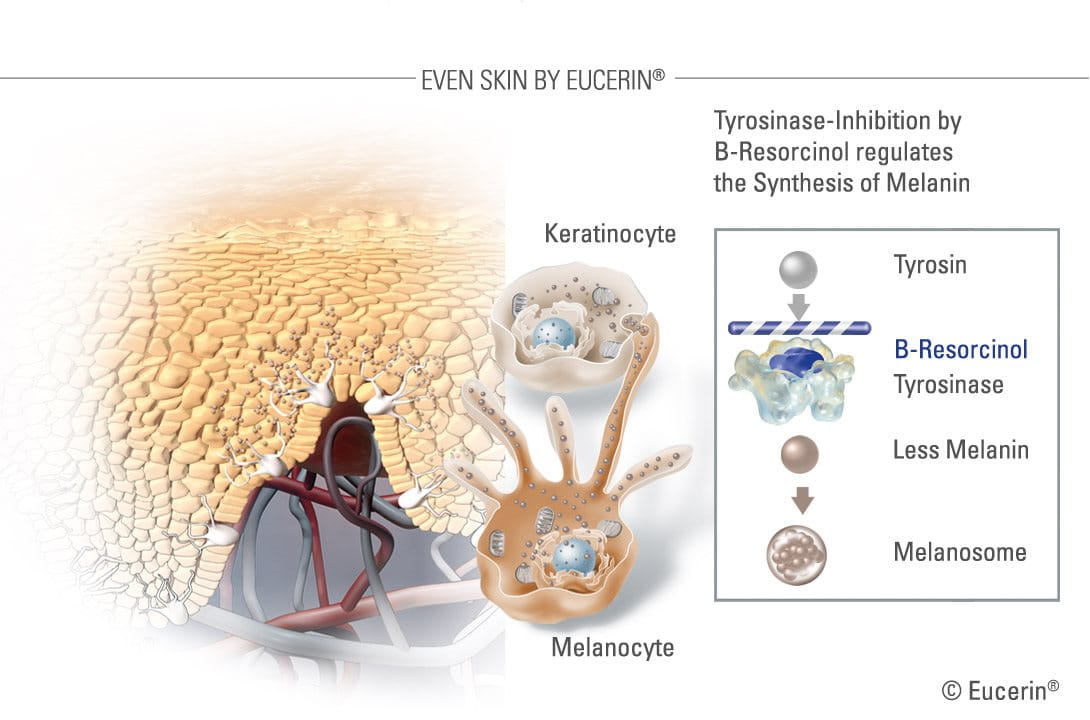
A very effective ingredient in reducing melanin production – and the main active ingredient in the Eucerin White Therapy range – is B-Resorcinol or butyl resorcinol. - B-Resorcinol has been clinically proven to start reducing dark spots in just four weeks. It is a very strong inhibitor of tyrosinase (the enzyme that forms melanin). It causes little to no skin irritation and is effective against the major kinds of hyperpigmentation, like melasma and age spots.


As well as the topical medical treatments, there are other considerations when managing melasma:
To prevent any further hyperpigmentation, it is recommended that those prone to melasma use broad-spectrum sunscreen with a high SPF every day as part of a daily cleanse, clear and care routine.
It does take some time for treatment to take effect – weeks rather than days - so be patient, consistent and persistent.
Attention
Talk to your dermatologist or pharmacist if any of your dark spots are new, have changed in appearance, or look different to your other spots.



