Post-inflammatory hyperpigmentation, commonly known as hyperpigmentation caused by inflammation, is a type of hyperpigmentation that can affect the face and body. It typically arises as a response to inflammation (such as acne, Atopic Dermatitis or Psoriasis) or injury (for example if triggered by dermabrasion, chemical peels or laser-therapies).


Post-inflammatory hyperpigmentation appears as flat spots of discolouration. These macules can range in colour from pink to red, brown or black, depending on skin tone and the depth of discolouration. They can resemble small, discoloured freckles or larger patches of darker skin and may be shiny or look like “new” skin.
PIH often affects people with acne and it can sometimes be triggered by aesthetic interventions such as dermabrasion, chemical peels or laser-therapies. All skin types can get post-inflammatory hyperpigmentation but it is more prevalent in darker tones of skin. In fact people with darker skin ask for advice from dermatologists on PIH more than any other condition. Men and women are equally susceptible to post-inflammatory hyperpigmentation.
Attention
If a pigment spot is changing in size, shape, colour, or is itching or bleeding, a dermatologist should be visited in order to rule out malignancy.
The signs, triggers and available treatments available for post-inflammatory hyperpigmentation
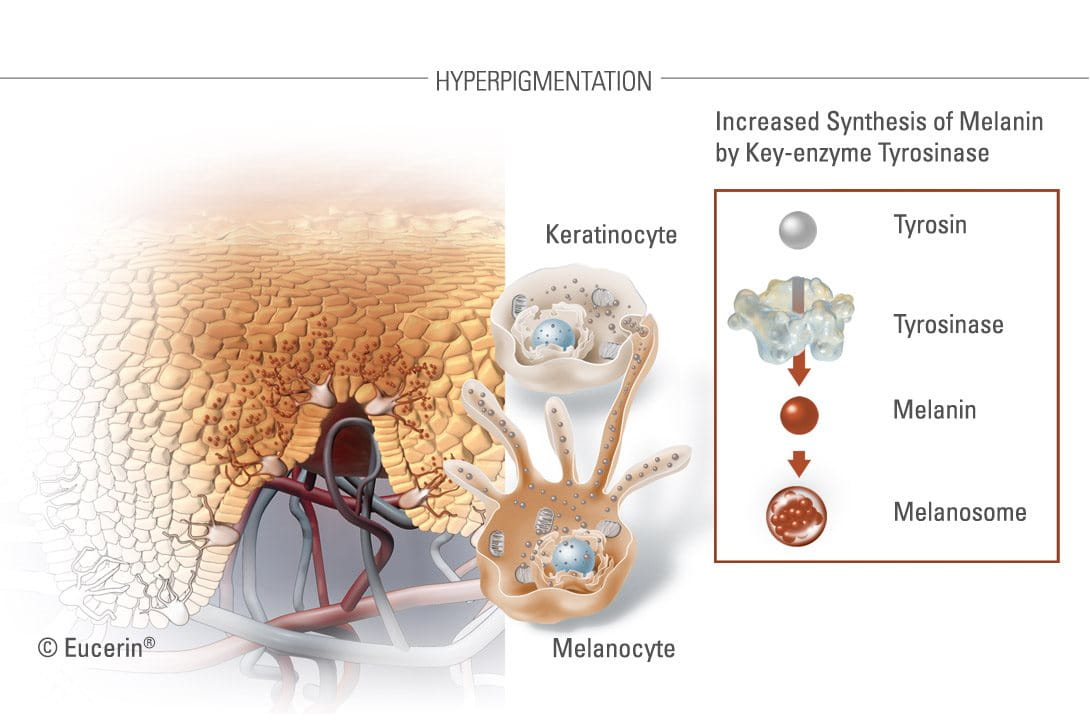
Hyperpigmentation occurs when internal or external factors cause an increase in melanin production. This results in discolouration of skin, most frequently on areas exposed to the sun. There are several forms of hyperpigmentation, like pigment spots (age spots and freckles), melasma and post-inflammatory hyperpigmentation (PIH).
What causes post-inflammatory hyperpigmentation?
When an injury, rash, spot or any other kind of influence causes skin to become inflamed, this inflammation triggers melanocytes - the melanin-producing cells – to release excessive melanosomes (pigment granules). These melansomes contain tyrosinase (a pigmentation enzyme that starts the melanin production) and synthesised melanin. Melanin is responsible for giving skin and hair its colour. The excessive pigment granules darken and discolour the formerly wounded area, remaining there long after the initial wound has recovered.


A post-inflammatory hyperpigmentation macule is often left behind as the result of an inflamed acne lesion.
PIH macules can appear from fairly insignificant papules or pimples right up to more serious wounds. That said, the more inflammation there is, the more obvious the PIH macule will be, both in terms of size and colour. If a pimple is squeezed or picked it will increase the chance of developing post-inflammatory hyperpigmentation.
Whilst not the cause of PIH, the sun can aggravate the symptoms, darkening the affected patches and prolonging the time it can take for them to fade.
Post-inflammatory hyperpigmentation does not cause scarring and, even with no treatment, it will improve over time. Recovery rates vary but, on average, it can take anything from three to 24 months for the darkened areas to fade. Although in some cases it may take longer. The timing depends on the difference in skin tone between the natural skin tone and the darkened patches - the more significant the difference, the longer it will take for the tones to rebalance. Treatments are available that can improve and speed up this recovery time.
What treatments exist for post-inflammatory hyperpigmentation?
There are two main concepts used by dermatologists: removal of the skin discolouration caused by post-inflammatory hyperpigmentation and regulation of the signs.
Removal
Removal – by laser-therapy, intense pulse list or chemical peel – deletes hyperpigmented skin cells to regenerate new, hyperpigmentation-free skin. It can be expensive, invasive and can actually make the condition worse. Potential side-effects include inflammation, irritation and a burning sensation.

Chemical peels eg. AHA
The dermatologist applies an acidic solution (Glycolic Acid (AHA)) to affected areas to remove layers of skin. Skin blisters at first, then peels to reveal “new”, unblemished skin underneath.
Laser-therapies (Fraxel, Erbium YAG) and Intense Pulse Light (IPL)
Laser-therapies and impulse light treatments tend to be more precise than chemical peels, as they use targeted high-energy lights to reach affected areas. Skin can be treated at surface (epidermis) level or deeper (dermis) depending on how severe the hyperpigmentation is. Read more about skin structure.
Regulation
Regulation uses prescription or over-the-counter remedies to inhibit melanin production and even skin tone, lightening darker patches so they match skin’s normal pigmentation.
There are a number of topical medical or skincare products available for post-inflammatory hyperpigmentation and these generally contain one or more of the following ingredients:
- Hydroquinone 2-4% (Rx only) - a powerful skin-bleaching agent that is banned in cosmetics in most parts of the EU due to concerns over links to potential toxicological risks. It is, however, still used in the US. Higher concentration (Rx >4%) is prescription-only while lower concentrations (>2%) are used in over-the-counter remedies.
- Arbutin is a key ingredient in many Asian skin-whitening products and a natural source of hydroquinone. Even though it is weaker, and less effective than industrially-produced hydroquinone, there are similar concerns about its safety.


- Kojic Acid is a by-product of the Japanese rice wine, sake. It is natural but its effectiveness at inhibiting melanin production is questionable and it has been banned in many countries.
- Glycolic Acid (or hydroxyacetic acid) is the acid used by dermatologists in chemical peels and it is a common active ingredient in many hyperpigmentation topical creams.
- Retinoic Acid has been seen to be effective but can trigger some side-effects including irritation and increased sun sensitivity (which is already an issue for people with post-inflammatory hyperpigmentation). As there have been some potential links to birth defects, pregnant or breastfeeding women should not apply Retinoid Acids.
- Vitamin C derivatives have also been proved to be relatively effective against post-inflammatory hyperpigmentation. They are often used in conjunction with other active ingredients.
B-Resorcinol
A very effective ingredient in reducing melanin production is B-Resorcinol or butyl resorcinol. It works by inhibiting tyrosinase, the enzyme that forms melanin. It is also the main active ingredient in the Eucerin White Therapy range.
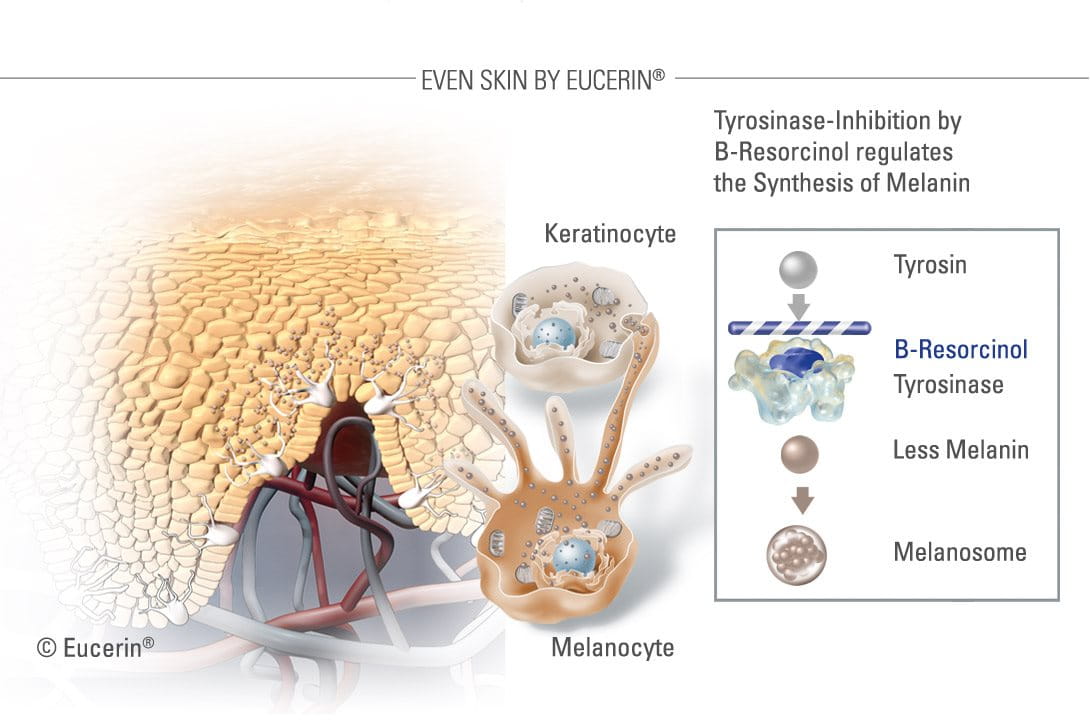
Eucerin White Therapy range, including B-Resorcinol, has been proven to start reducing dark spots in just four weeks. It causes little to no skin irritation.
Sufferers of post-inflammatory hyperpigmentation should also be aware that:


- The sun’s UV-rays are a major influence on skin. Sun exposure is likely to exacerbate symptoms so, as well as trying to avoid sun, it is recommended that a broad-spectrum, high factor sunscreen is applied every day as part of a daily cleanse, clear and care routine.
- There are overnight results to be expected. Treatments may take several weeks before any noticeable difference so consistency, patience and persistence are very important.
- Post-inflammatory hyperpigmentation may require medical care. If sufferers are concerned about the size, shape or colour of any dark patches, it is worth consulting a dermatologist or pharmacist.




